Hepatitis B (HBV) is more than just a viral infection—it’s a stealthy assailant that can damage your liver over time, often without obvious symptoms. If you’re wondering how hepatitis B damages the liver, what the stages are, and how to prevent irreversible harm, this post breaks it down clearly.
Hepatitis B is widely recognised as a “silent killer,” lurking within the liver and devastating its function long before symptoms appear or damage is noticed. This viral infection quietly infiltrates liver cells, triggering a relentless battle with the body’s immune system that causes ongoing inflammation, scarring, and—if left unchecked—irreversible harm such as cirrhosis or even cancer. Facing hepatitis B means confronting more than just the physical implications of the virus; it requires courage and awareness to deal with its emotional toll, its stigma, and the profound fear of what it can do over time within the body’s most vital filter: the liver.
What Is Hepatitis B and Why Does It Matter
Hepatitis B is caused by the hepatitis B virus, which infects liver cells (hepatocytes). It can be an acute infection (short-term) or become chronic, meaning the virus persists for more than six months. Around the world, chronic HBV is a major cause of liver cirrhosis and liver cancer. (World Health Organisation)
Transmission occurs through infected blood or body fluids, such as through unprotected sex, contaminated needles, or vertical transmission (mother to child at birth). (World Health Organisation)
How Hepatitis B Damages the Liver: The Mechanism
Here is how HBV results in liver damage:
- Viral replication and infection of hepatocytes
Once HBV enters the body, it infects liver cells and begins replicating. These infected cells display viral antigens, which signal the immune system. (British Liver Trust) - Immune response and inflammation
The body’s immune system tries to eliminate infected cells. This immune attack causes inflammation in the liver. Over time, repeated inflammation injures both infected and nearby healthy liver tissue. (British Liver Trust) - Fibrosis
With ongoing inflammation, liver tissue tries to heal. But healing involves laying down scar tissue when damage is frequent. This scarring, or fibrosis, reduces the liver’s ability to function normally. (British Liver Trust) - Cirrhosis and structural damage
As fibrosis becomes more widespread, the liver architecture changes: nodules form, blood flow becomes disrupted, and the organ becomes stiff. Cirrhosis is essentially severe scarring. This reduces function, increases pressure inside portal veins, and leads to complications such as ascites, variceal bleeding, and hepatic encephalopathy. (NIDDK) - Liver cancer (Hepatocellular carcinoma, HCC)
Chronic inflammation and continuous cell regeneration increase the chances of DNA damage in hepatocytes. HBV itself can integrate its DNA into host liver cells, potentially triggering oncogenesis. Thus, even without full cirrhosis, there is an elevated cancer risk. (NCBI)
Stages of Hepatitis B Liver Damage
Medical professionals often consider several phases (or “stages”) in chronic HBV infection. According to the British Liver Trust and other sources, these stages include: (British Liver Trust)
| Stage | What Happens |
| Immune tolerance | Virus replicates actively, but the immune response is weak. Minimal liver damage initially. |
| Immune active | The immune system begins attacking infected cells; inflammation and liver injury increase. Elevated ALT (liver enzyme), high viral replication. |
| Inactive carrier / low replicative | Virus replication lowers or becomes inactive. ALT levels normalise; less inflammation. But the virus is still present. |
| Reactivation | The virus becomes active again after a period of inactivity. Inflammation, viral load increase. |
| Advanced disease / Complications | Progress to significant fibrosis, cirrhosis. Possible liver failure or cancer. |
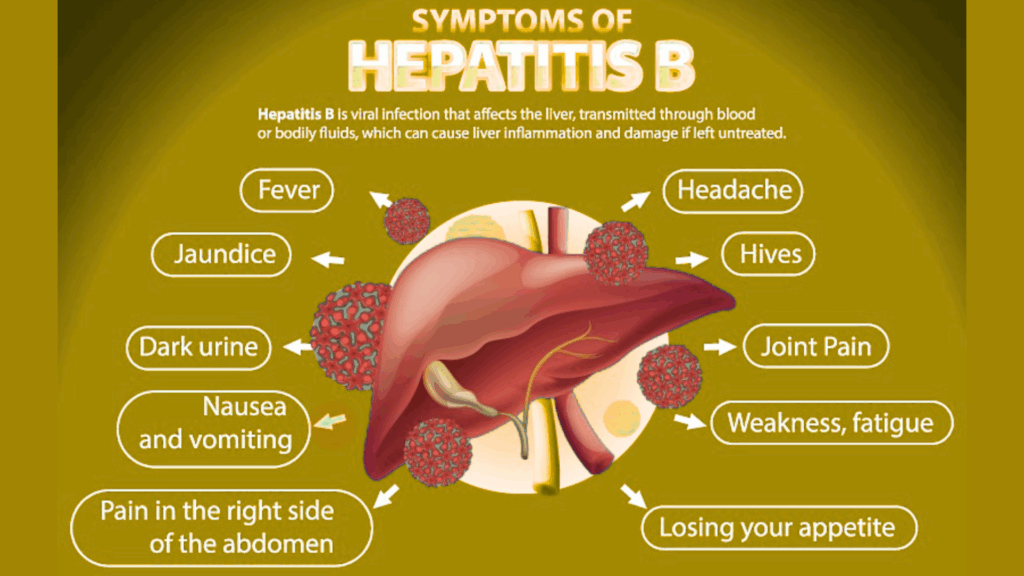
Signs & Symptoms
Early stages may show no symptoms. When symptoms do appear, they often include:
- Fatigue, weakness, loss of appetite
- Nausea, vomiting
- Pain or discomfort in the upper right abdomen
- Jaundice (yellowing of skin and eyes)
- Dark urine, pale stools (Mayo Clinic)
When damage becomes severe (cirrhosis or cancer), symptoms may include: abdominal swelling, fluid retention, bleeding from varices, confusion, etc. (NCBI)
Risk Factors That Speed Up the Damage Of Hepatitis B
Some people are likely to have faster progression or more severe damage. Key risk factors:
- Infection at birth or early childhood
- High viral load with persistent replication
- Co-infections (HIV, hepatitis C, D, etc.)
- Alcohol use, obesity, fatty liver disease
- Weak immune system (e.g. medications, illness)
- Genetic factors & male gender (NCBI)
Prevention & Treatment: Halting the Damage
It’s possible to prevent most HBV-related liver damage. Here’s how:
- Vaccination: This is the key to prevention. The HBV vaccine is safe, efficacious, and safe for infants, children, and adults who have never been vaccinated.
- Screening & early detection: Blood testing, such as HBsAg, HBV DNA, liver enzymes such as ALT, ultrasound, etc., is done to quantify the viral activity and liver damage. Early detection allows for early intervention.
- Antiviral therapy: In long-term cases, medication (tenofovir, entecavir) can suppress HBV replication and inflammatory processes, slow down or reverse fibrosis and decrease the risk of cirrhosis and cancer.
- Lifestyle modifications: Avoid alcohol, maintain a healthy weight, and manage existing liver conditions.
- Continuous monitoring: Such patients should be under regular follow-up by liver specialists. Comprehensive follow-up and management of such patients is available at the clinic of Dr Vrishit Saraswat — details available on his HBV treatment page.
When Damage Becomes Deadly
Left unchecked, hepatitis B may lead to:
- Liver failure: When the liver can no longer perform essential functions.
- Cirrhosis complications: Portal hypertension, internal bleeding, ascites, and encephalopathy.
- Liver cancer (HCC): Risks increase after long-term chronic infection and advanced fibrosis.
- Death: From complications such as bleeding, infection, liver failure, or cancer. (NCBI)
What You Should Do:
If you suspect you may have been exposed to HBV, or you are at high risk:
- Get tested: Do HBV serology, viral load, and liver function tests.
- Vaccinate if you are not already: Especially for infants, healthcare workers, and people in high-risk groups.
- Seek expert care: A gastroenterologist/hepatologist can guide antiviral therapy and monitor liver health. Dr Rishi Saraswat is skilled in diagnosing, treating, and managing chronic HBV. Check out his clinic’s “About” page for credentials and how to book a consultation.
- Maintain a healthy lifestyle: Good nutrition, avoid liver toxins, stay hydrated, and manage comorbidities.
Final Thoughts
“How Hepatitis B Damages the Liver” isn’t just a phrase—it reflects a very real, preventable path of illness that many people endure silently. With early detection, vaccination, expert care, and lifestyle choices, the damage can often be slowed or avoided.
For trusted expert consultation, liver health evaluation, or treatment decisions, you can rely on Dr Vrishit Saraswat’s practice. Together, let’s bring awareness, act early, and protect the liver.
References & Further Reading
- World Health Organisation: Hepatitis B fact sheet (World Health Organisation)
- Mayo Clinic – Symptoms & Causes of Hepatitis B (Mayo Clinic)
- British Liver Trust – Stages of HBV infection & liver damage (British Liver Trust)
- CDC – Clinical overview & long-term effects (CDC)
FAQs
Q1. Can hepatitis B be cured completely?
No, chronic hepatitis B cannot be fully cured, but it can be controlled with antiviral medications. In some cases, the infection clears naturally if it’s acute.
Q2. Can hepatitis B patients live long?
Yes, with proper treatment, monitoring, and a healthy lifestyle, many hepatitis B patients can live a normal lifespan.
Q3. Is hepatitis B serious?
Yes, untreated hepatitis B can cause serious complications like liver damage, cirrhosis, and even liver cancer.
Q4. Is Hep B a genetic disease?
No, hepatitis B is not genetic. It is a viral infection transmitted through blood, body fluids, or from mother to child at birth.
Q5. Is hepatitis B cancerous?
Hepatitis B itself is not cancer, but chronic infection increases the risk of developing liver cancer (hepatocellular carcinoma).