Understanding the Challenge of Osteoarthritis

Osteoarthritis is the most common type of arthritis. It’s a long-term joint disease that causes the cartilage—the smooth tissue that cushions joints—to wear down over time. As the condition progresses, bones can rub against each other, causing pain, stiffness, and swelling, especially in the knees and hips.
Traditional treatments include:
- Weight loss
- Physiotherapy
- Pain medications (like NSAIDs)
- Corticosteroid injections
While these methods may provide short-term relief, they often fail to stop the disease from getting worse. Many patients eventually face total knee replacement (TKR), but:
- Some can’t undergo surgery due to other health issues
- Others fear a long recovery time
- Up to 20% of patients remain dissatisfied even after surgery
Because of these limitations, doctors are turning to a new approach: Interventional Radiology (IR).
Interventional Radiology: A New Hope for Osteoarthritis Relief
Interventional Radiology uses image-guided, minimally invasive procedures to treat osteoarthritis pain with pinpoint accuracy. These techniques offer faster recovery, fewer side effects, and targeted relief.
Medanta: Interventional radiology offers minimally invasive OA solutions. (@Medanta)
Let’s explore the leading options.
Image-Guided Injections: Targeting the Pain
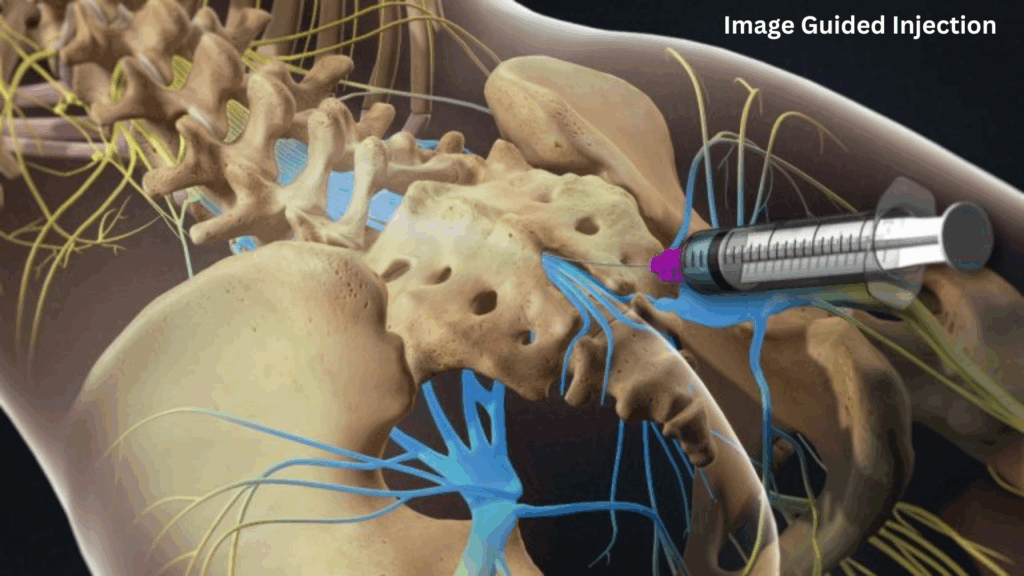
IR procedures use ultrasound or fluoroscopy to guide injections directly into the painful joint. This real-time imaging improves both safety and accuracy.
Common injection therapies include:
- Corticosteroids – for fast pain relief
- Hyaluronic Acid (Viscosupplementation) – adds lubrication to the joint
- Platelet-Rich Plasma (PRP) – promotes healing using your own blood
- Mesenchymal Stem Cells (MSC) – potential for long-term repair
While corticosteroids are well-known, PRP and MSCs show promise for regeneration, though more research is still needed.
Emerging use of GAE in knee OA management. (Diagnostic Imaging)
Neuroablative Techniques: Shutting Down the Pain
In osteoarthritis, pain often comes from sensory nerves around the joint. With radiofrequency ablation (RFA), IR doctors can safely “turn off” these pain signals.
How RFA Works:
- A probe is guided to the genicular nerves (around the knee)
- Heat is applied to “ablate” the nerve
- Pain relief can last 6 to 24 months
Compared to steroid injections, RFA offers longer-lasting relief and less tissue damage.
Genicular Artery Embolisation (GAE): Cutting Off Pain at the Source
One of the most exciting IR treatments is Genicular Artery Embolisation (GAE). This method targets the tiny blood vessels that feed the inflamed joint.
How GAE Works:
- A small catheter is inserted (usually through the groin or wrist)
- Using imaging, it’s guided to the genicular arteries in the knee
- Tiny beads (embolic agents) are injected to block these vessels
- Inflammation is reduced, and pain relief follows
Results That Matter:
- 99.7% success rate in performing the procedure
- 78%–92% of patients report major pain and function improvement
- Relief can last up to 2 years
- Side effects are rare and usually mild (like temporary skin changes)
GAE is ideal for patients who:
- Are not candidates for surgery
- Want to delay joint replacement
- Need a quicker recovery (just 1–2 days)
The Future of Osteoarthritis Treatment: AI + Personalisation
New technology is taking osteoarthritis care even further:
- AI and deep learning now help read X-rays and MRIs faster and more accurately
- Personalised treatment plans based on imaging, biomarkers, and disease severity
- Smart tools may soon predict which IR method (like GAE or RFA) will work best for each patient
Real Results: Dr Vrishit Saraswat’s Interventional Radiology Clinic
At the forefront of this innovation is Dr Vrishit Saraswat, offering state-of-the-art interventional radiology services. His clinic focuses on:
- Minimally invasive treatments
- Precision pain relief
- Patient-first care
From PRP injections to GAE and RFA, each treatment is tailored to your needs.
👉 [Explore Our Services] or [Contact Us] to learn more or book a consultation.
Why Interventional Radiology is a Game-Changer for Osteoarthritis
| Advantage | What It Means |
|---|---|
| Minimally Invasive | Lower risk, faster recovery, and usually done as an outpatient |
| Targeted Treatment | Accurate delivery of medication or therapy right where it’s needed |
| Delay or Avoid Surgery | Perfect for patients who can’t or don’t want joint replacement |
| Long-Lasting Relief | GAE offers up to 2 years of relief; RFA provides relief for several months |
| Smart & Personalised | AI and advanced imaging help choose the best treatment for each individual |
In Summary
Osteoarthritis doesn’t have to mean constant pain or immediate surgery. With interventional radiology, patients now have access to advanced, targeted treatments like GAE and RFA that offer:
- Faster relief
- Less downtime
- Better outcomes
As AI and imaging tools evolve, the future of osteoarthritis care is becoming smarter, safer, and more personal.
Ready to explore your options?
👉 Talk With Us today and see if interventional radiology can be your path to pain-free living.
FAQs
❓ How to relieve severe osteoarthritis?
Severe osteoarthritis can be managed through a combination of treatments. Lifestyle changes such as weight management, regular low-impact exercises (like swimming or walking), and physical therapy can help reduce joint stress. Medications such as pain relievers, anti-inflammatory drugs, or corticosteroid injections may provide relief. In advanced cases, interventional radiology procedures or joint replacement surgery may be recommended to restore mobility and reduce pain.
❓ What is the most painful stage of osteoarthritis?
The most painful stage of osteoarthritis is usually the late stage (Stage 4). At this point, the protective cartilage is almost completely worn away, leading to bone-on-bone friction, chronic inflammation, stiffness, and significant pain even during rest. Daily activities such as walking, bending, or climbing stairs become extremely difficult.
❓ What deficiency causes osteoarthritis?
While osteoarthritis is mainly caused by cartilage wear and tear, certain deficiencies can worsen it. Low levels of Vitamin D and Calcium are linked to weaker bones and poor joint health. Additionally, Vitamin C deficiency can impair collagen production, which is essential for cartilage repair. Maintaining proper nutrition helps slow the progression of osteoarthritis.
❓ What is the root cause of osteoarthritis?
The root cause of osteoarthritis is the breakdown of cartilage that cushions the ends of bones in the joints. Over time, this wear and tear leads to joint inflammation, stiffness, and pain. Risk factors include ageing, obesity, previous joint injuries, genetic predisposition, and overuse of joints due to repetitive activities.
❓ Which is worse, osteoarthritis or osteoporosis?
Both conditions affect bone and joint health, but in different ways. Osteoarthritis causes joint pain, stiffness, and mobility issues due to cartilage breakdown, while osteoporosis leads to fragile bones and a higher risk of fractures. Which condition is “worse” depends on the individual—osteoporosis may be more dangerous due to fracture risks, but osteoarthritis often causes more chronic pain and mobility limitations.