What happens during a breast tumour localisation procedure
What is breast tumour localisation and why does it matter
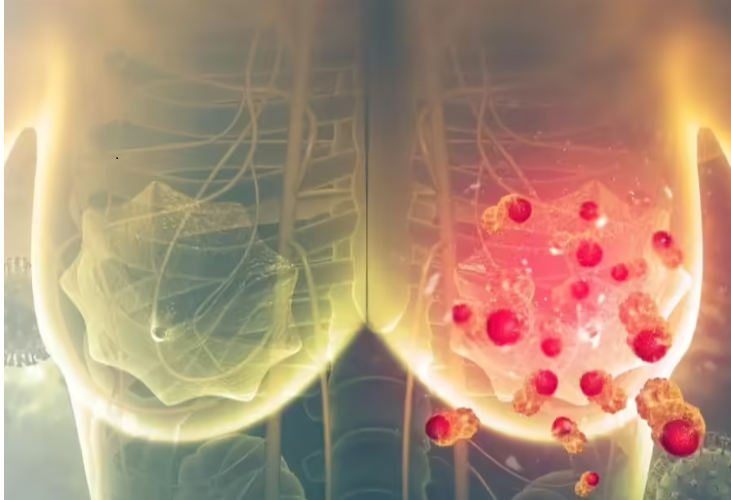
An abnormal mass or growth of cells in the breast tissue is a breast tumour. Tumours can be distinguished as “benign (non-cancerous)” or “malignant (cancerous)”. A benign tumour is mostly harmless, but there are times when it has to be removed due to pain or growth. On the other hand, malignant breast tumours are cancerous and could spread to other parts of the body if left untreated. Early detection through screening, mammograms, and self-exams is critical because it greatly enhances the patient treatment outcome and long-term survival.
Many early breast cancers are too small to feel by hand (non-palpable). Before breast-conserving surgery (lumpectomy), radiologists “localise” the lesion using imaging so surgeons can remove the right tissue with clear margins while preserving healthy breast tissue. Historically, this was done with a thin guidewire placed under mammography or ultrasound on the day of surgery, a method known as wire-guided localisation (WGL). Newer, wire-free options now offer more flexibility and comfort without sacrificing accuracy. (PMC)
The main image-guided localisation options
- Wire-guided localisation (WGL): A fine wire is inserted so the tip sits at or just beyond the lesion. Surgeons follow the wire path during surgery. It’s effective but ties placement to the day of surgery, can be uncomfortable, and may restrict incision planning. (PMC)
- Magnetic seed localisation (e.g., Magseed®, MOLLI): A rice-sized metal marker is placed under ultrasound or mammography and later detected with a handheld magnetic probe in theatre. Seeds can be placed days to months in advance, easing scheduling and often improving cosmetic incision choice. (PMC)
- Radar reflectors (e.g., SAVI SCOUT®): A tiny reflector is implanted and located intra-operatively with a console and probe that reads radar signals no radiation involved. (Applied Radiology)
- Radioactive seed localisation (RSL): A small I-125 seed is placed and detected during surgery with a gamma probe; widely studied and considered clinically equivalent to wire localisation in outcomes in many settings. (Handled under specific radiation safety protocols.)
- MRI-guided wire localisation: For lesions visible only on MRI, wires can be placed using MRI guidance to ensure accurate removal. (PMC)
Know more about our services http://drvrishitsaraswat.com/our-services/
What the latest evidence shows
A large comparative review found wireless techniques (SAVI SCOUT, radioactive seed, and radioguided occult lesion localisation) were associated with lower positive margin and re-excision rates compared with WGL. For example, pooled data comparing SAVI SCOUT vs. WGL showed fewer re-excisions (8.6% vs 18.8%). (PMC)
Magnetic seeds are reliable even when placed well before surgery; studies report 100% retrieval and stable positioning over extended intervals after neoadjuvant therapy, supporting flexible, patient-friendly scheduling.
Newer magnetic systems (e.g., MOLLI) also show high placement accuracy and retrieval success in real-world cohorts, reinforcing wire-free localisation as a robust alternative. (Arch Breast Cancer)
How your care team chooses a localisation method
Your care team selects a localisation method according to tumour size, location, imaging visibility, and your health condition. Wires, seeds, markers, or imaging guidance may be used to visualise the tumour accurately. This is meant for the safe removal of the tumour while preserving healthy tissue and increasing the accuracy of the surgical intervention.
Your radiologist and breast surgeon consider:
- Lesion visibility (ultrasound vs mammography vs MRI only)
- Breast-conserving plans and incision placement for the best cosmetic result
- Clinic logistics (same-day vs prior placement)
- Radiation rules (if using RSL)
- Presence of a clip placed at biopsy, and whether bracketing is needed for larger or multiple targets
The goal is the same: accurate removal with clear margins while preserving healthy tissue, echoed by current resource guides on margins in breast-conserving surgery.
What can patients expect on the day?
- Placement (if same-day): You’ll have local anaesthetic; imaging guides the precise placement of the wire/seed/reflector.
- Surgery: The surgeon uses a detector (for seeds/reflectors) or follows the wire to remove the target with a rim of normal tissue.
- Pathology: Margins are checked. If tumour cells are seen at the edge (a “positive margin”), a re-excision may be advised, something modern localisation aims to reduce.
Advantages of wire-free localisation
- Scheduling freedom: Devices can be placed before surgery, reducing day-of-surgery stress.
- Incision planning: Surgeons aren’t constrained by a protruding wire, which can help cosmetic outcomes.
- Comfort and workflow: No external wire; operating theatres can run more smoothly.
FAQs
1- Where is the most common location for a breast tumour?
Most breast tumours are found in the upper outer quadrant of the breast, in the vicinity of the armpit. In that area, the largest bulk of breast tissue is available for the cleavage of tumours.
2-How to know if a breast lump is cancerous?
A malignant breast lump tends to be hard, irregularly shaped, and fixed to surrounding tissue as opposed to benign lumps, which feel smooth and can be moved. However, medical tests such as a mammogram, ultrasound, and biopsy are needed for a diagnosis of cancer in a lump.
3- Is wire-free localisation as accurate as wire localisation?
Yes. Multiple studies and reviews show comparable or better margins and re-excision outcomes with wireless devices, depending on the technique and case selection.
4- What does a cancerous tumour feel like in a breast?
A cancerous breast tumour usually feels like a hard, firm lump with uneven or irregular borders. It may feel fixed in place and often does not hurt; however, some people may feel discomfort. Regular screening is essential because not all cancer lumps can be palpated easily.
5- Can localisation be done if I had chemo first?
Yes. Seeds can mark the tumour bed before treatment and remain detectable for months, guiding surgery after tumour shrinkage.